PAN is associated with hepatitis B and other viral infections. Diagnostic clues include the presence of systemic features, such as fever, malaise, weight loss; ischemic symptoms, including myalgia, renovascular hypertension, severe abdominal pain, testicular pain, livedo reticularis and digital gangrene; and symptoms secondary to ruptured aneurysms, including intra-abdominal and renal hemorrhage.
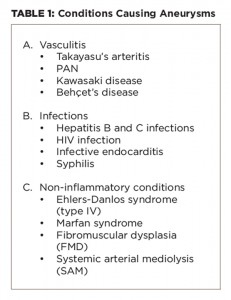
It’s imperative to also consider important differential diagnoses that cause aneurysms, including other types of small and large vessel vasculitis, infections and non-inflammatory vasculopathies, because treatment differs according to the cause.
Important differential diagnoses that cause aneurysms are given in Table 1.
Aneurysms occur in the other forms of vasculitides, as well. In Takayasu’s aortoarteritis (large vessel vasculitis), aneurysms are well described in the aorta and its major branches in the proximal portions of these vessels on angiography, and rarely, there are aneurysms of the visceral arteries.4 It usually presents with limb claudication, CNS ischemic symptoms, absent or unequal pulsations and hypertension. Pulmonary artery aneurysms presenting in the midpart of the pulmonary artery, presenting with hemoptysis is typical of Behçet’s disease (variable vessel vasculitis) and is associated with the predominant mucocutaneous and ocular features.1 Kawasaki disease (medium vessel vasculitis) is characterized by coronary artery aneurysms in children.1
Non-inflammatory vasculopathies can cause aneurysms, which could be asymptomatic. They include fibromuscular dysplasia (FMD), systemic arterial mediolysis (SAM), Marfan syndrome and Ehlers-Danlos syndrome (EDS) type IV.5
FMD typically affects young females, preferentially affects renal arteries with string of bead appearance on angiography and may be asymptomatic or may lead to hypertension. However, isolated intra-parenchymal renal aneurysms are rare in FMD. Similarly, in Marfan syndrome the aorta is predominantly affected by aneurysms and dissection of the involved vessels, and other clinical features are present. In EDS type IV, aorta, celiac artery, splanchnic vessels and renal vessels are most commonly affected. Again, the lesions in EDS are more proximal, with increased risk of aneurysms, dissections and rupture.
It’s imperative to also consider important differential diagnoses that cause aneurysms, including other types of small & large vessel vasculitis, infections & non-inflammatory vasculopathies.
Back to the Case
In our patient, there were no clues (i.e., clinical, laboratory or imaging) to suggest these other differentials. Although there were no other clinical features of PAN and the inflammatory markers were normal, the diagnosis of PAN was tenable.2
Although there were no other clinical features of PAN—the inflammatory markers were normal and viral serologies were negative—in the view of hypertension, presence of multiple intra-renal and splenic aneurysms on CT angiography, abdominal hemorrhage and response to immunosuppressive treatment, the diagnosis of PAN was tenable.2,6-8