
Image Credit: Lightspring/shutterstock.com
In diagnosing and treating a disease that is rapidly gaining recognition worldwide since it was first recognized in Japan in 2003, 42 experts from 10 different countries recently collaborated to discuss and review the current experience and data on IgG4-related disease.
The result is the “International Consensus Guidance Statement on the Management and Treatment of IgG4-Related Disease,” published in July 2015 in Arthritis & Rheumatology.1
A Systemic Disorder
Defined as a fibroinflammatory condition mediated by the immune system that can affect multiple organs and lead to tumefactive, tissue-destruction lesions and organ failure, IgG4-related disease is now recognized as a systemic disorder that links many individual organ conditions once thought not to be related.1
Diagnosis is complicated by the many conditions that can mimic the disease. The disease is often mistaken for a malignancy, an infection or other immune-mediated conditions, such as Sjögren’s syndrome, giant cell arteritis or granulomatosis with polyangiitis.
“IgG4-related disease is an emerging systemic condition linking many disorders once regarded as isolated, single-organ conditions that were managed by different subspecialties,” says Arezou Khosroshahi, MD, assistant professor of medicine, Rheumatology Division, Emory University School of Medicine, Atlanta, and lead author of the study. “Most patients with IgG4-related disease undergo multiple invasive procedures for suspected malignancy before the diagnosis is considered, which delays their diagnosis and on-time treatment.”
According to Dr. Khosroshahi, the disease has only been recognized in the U.S. in the past decade and published evidence on the disease is still quite thin, with no prospective, randomized trials yet available.
Given the rapid recognition of the disease within the past decade, however, experts felt some guidance was needed to help clinicians diagnose and manage a complicated disease that can affect multiple organs, most commonly the pancreas, biliary tract, major salivary glands, lacrimal glands, retroperitoneum and lymph nodes. Indeed, because of the widespread anatomical areas in which the disease can present, experts representing eight specialties (i.e., gastroenterology, rheumatology, ophthalmology, pulmonary-critical care, hematology/oncology, internal medicine, nephrology and endocrinology) were among the experts included in the development of the consensus statement.
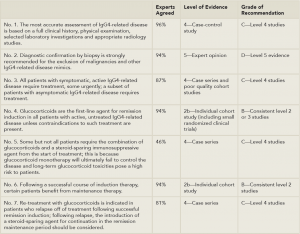
(Click for larger image)
Table 1: 7 Key Consensus Statements
Adapted and compiled from References 1 and 2.
The consensus statement offers clinicians seven key statements to help guide diagnosis and treatment of IgG4-related disease (see Table 1). The primary evidence available and used to base these statements on came primarily from individual small cohorts, case series and expert opinions in the literature, according to Dr. Khosroshahi. Each statement is accompanied by the percentage of experts who agreed with the statement, along with the quality of evidence based on the Oxford Centre for Evidence-Based Medicine (OCEBM), in which the level of evidence is graded from 1a-5 (1a being the best quality of evidence) and grade of recommendation ranges from A (strongest recommendation) to D (lowest).2 (For more information on the OCEBM grading system.)


