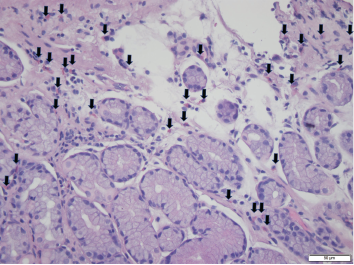
Foci of increased eosinophils (arrows) in superficial layers of the stomach (hematoxylin and eosin stain at 40X magnification).
Eosinophilic gastroenteritis (EGE) is a rare condition caused by eosinophilic infiltration of the gastrointestinal (GI) tract. The condition is subdivided into the GI layers it affects: mucosal, muscular and subserosal.1 EGE usually presents with non-specific GI symptoms, such as impaired motility, intestinal obstruction and, rarely, ascites.2
Below, we report a rare case of EGE leading to eosinophilic ascites associated with rheumatoid arthritis (RA).
The Case
A 57-year-old man with RA presented to an outpatient GI clinic. He complained of abdominal distension and bloating and said he’d been experiencing these symptoms for the past few years. The patient reported passing large amounts of gas, but denied any pain or bleeding with defecation, nausea, vomiting, diarrhea or constipation. He had not experienced any pain or difficulty on swallowing, reflux or burning sensation after meals. He had no fever, chills or weight loss, and was not taking aspirin or non-steroidal anti-inflammatory drugs (NSAIDs). His vital signs were stable.
When the patient initially presented with his abdominal complaints, he was taking 20 mg of leflunomide once daily for his long-standing RA. He had previously taken prednisone for his RA flares, but was not on steroids at the time of presentation. He had no surgeries. He did say he was allergic to naproxen, which caused angioedema. He did not smoke, or use alcohol or recreational drugs.
A physical exam revealed a soft, non-tender, distended abdomen with a positive fluid wave. Lab tests revealed normocytic anemia and an elevated erythrocyte sedimentation rate of 76 mm/hr (normal: 0–20 mm/hr), likely secondary to his RA. His white cell count was 5.22 K/uL (normal: 3.50–10.80 K/uL), with a normal eosinophilic count. The patient had previously been worked up extensively at another hospital, where a liver biopsy was performed, but was reportedly unremarkable.
An abdominal ultrasound showed moderate ascites and mild hepatomegaly. A diagnostic paracentesis was performed, which revealed ascites albumin 2.6 g/dL, total protein 4.7 g/dL, glucose 99 and lactate dehydrogenase 178. Serum albumin was 3.66 g/dL (normal: 3.5–5.70 g/dL) . Calculated serum ascites albumin gradient (SAAG) is the current method to determine the etiology of ascites (replaced the outdated method of transudate and exudate fluid classification). We calculated the SAAG to be 1.06 g/dL ([serum albumin 3.66 g/dL] – [ascitic albumin 2.6 g/dL]). This is <1.1, which suggests a peritoneal etiology for this ascitic fluid and rules out portal hypertension (SAAG >1.1). An analysis of the patient’s peritoneal fluid revealed 1,077 white blood cells (0–100/uL), with 28% eosinophils and 29% lymphocytes. There was no evidence of malignant cells, although reactive cellular changes were noted.
A cardiac etiology of the ascites was ruled out with an echocardiogram, which showed an ejection fraction of 65% and no evidence of pericardial effusion. A hepatic etiology to his ascites was thought to be unlikely due to the serum-ascites albumin gradient, normal liver ultrasound, normal liver function tests and prior liver biopsy. Leflunomide was considered a possible cause of the ascites, but upon chart review, the patient had ascites before he started leflunomide therapy. Further, the patient noted that starting leflunomide therapy did not exacerbate his GI symptoms.
Due to the unclear etiology of the ascites, a computed tomography (CT) scan was performed on his abdomen, which revealed dilated small bowel loops, suggestive of small bowel obstruction, mesenteric lymphadenopathy and hepatomegaly. Shortly thereafter, the patient experienced an RA flare and was started on 20 mg of prednisone daily.
A few months later, the patient followed up in our GI clinic and was asymptomatic, with only occasional dyspepsia after eating spicy foods and occasional loose stools. The patient subsequently underwent an esophagogastroduodenoscopy, which revealed gastropathy with atrophic antral mucosa, periampullary diverticulum and patulous pylorus. Random biopsies from the stomach were taken and noted to contain eosinophils throughout, with foci up to 35 eosinophils per high power field (HPF) examination (see Figure 1, left). A colonoscopy proved unremarkable.
At this point, due to the stomach biopsies and ascitic fluid analysis, a diagnosis of eosinophilic gastritis and ascites was reached. Because the patient was asymptomatic and had already been started on 20 mg prednisone daily for his RA, the dosage was not increased. The patient remained asymptomatic at subsequent follow-up.



