Given the presence of thickened cracked skin on the patient’s hands, which we felt to be consistent with mechanic’s hands, negative ANA, positive cytoplasmic and Ro antibodies, as well as history of Raynaud’s phenomenon and arthralgias, an antisynthetase syndrome was considered. A myositis-specific antibody panel was sent.
The patient then underwent a right upper-lobe wedge biopsy. This showed acute and organizing diffuse alveolar damage (DAD) with marked cytologic atypia, vascular thrombosis, collections of eosinophils, and vascular mural thickening. Hyaline membranes involved most of the specimen (see Figure 3). Immunohistochemistry for HSV showed a rare, weakly positive cell but no characteristic viral cytopathic inclusions. Immunohistochemistry for cytomegalovirus was negative. No organisms were seen on Grocott’s methenamine silver stain (GMS), AFB, Brown-Hopps, or Steiner stains. There was no evidence of malignancy.
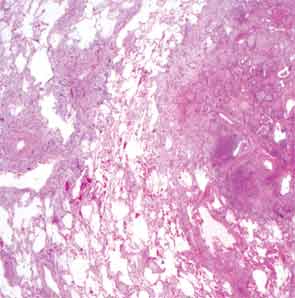
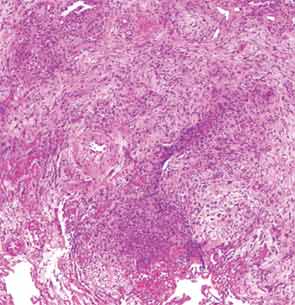
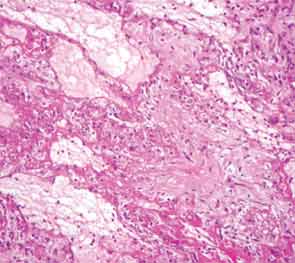
The overall picture was that of an acute alveolar injury in an exudative and fibroproliferative phase, superimposed on an older process with organizing pneumonia by perhaps two to three weeks. Some lymphoid aggregates were suggestive of possible autoimmune etiology.
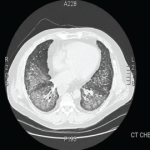
His lung biopsy was complicated by pneumothorax (see Figure 4). He required multiple chest tube placements. He underwent a tracheostomy procedure.
In mid January, two days after his lung biopsy, pulsed dose steroids were started, 1 g solumedrol IV daily for three days, followed by prednisone 60 mg daily. He was continued on acyclovir for prophylaxis for HSV reactivation. Because of persistent fevers, broad-spectrum antibiotics were resumed. Cyclophosphamide was considered, however, at the time, stains for pathogens from his lung biopsy were still pending. In this setting we worried about the added risk that a broad immunosuppressive approach with cyclophosphamide was going to pose and we chose instead to treat the patient with B-cell depletion only. He was thus started on rituximab and received 1 g IV on Day 2 of his pulsed steroid dose. A second dose of 1 g IV was given two weeks later. His respiratory status began to improve three days after the start of the immunosuppressive treatment. Over the ensuing week, he went on to have a dramatic clinical response and was able to wean off of ventilator support completely eight days after initiation of immunosuppressive treatment. The myositis-specific antibody panel returned positive for PL-7.