Reassessment of outcomes in July 2008 showed that the redesign led to reductions in cost, both in terms of reduced hospitalizations (by 11.7%) and monthly Medicare spending (by $217 per enrollee).
“Our results show that delivering the right care management program to the right people can work,” write the investigators. “Serving high-risk patients with an intervention that incorporates strong transitional care, medication management, systematic assessments, focused care plans and the opportunity for in-person contacts by care managers with patients and providers reduced hospitalizations and Medicare spending.”6
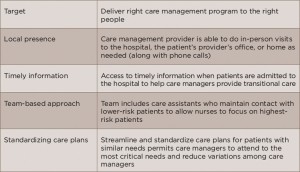
(click for larger image) Table 4: Issues to Consider in Developing a Successful Care Program
Source: Adapted from reference No. 6.
Table 4 (right) lists a number of implications from the redesign of the WUSM care program that echo the suggestions provided in Tables 2 and 3 in implementing a successful care program.
Ongoing Challenges
Despite the success of these features and their implementation in improving patient outcomes, both Dr. McCarthy and Dr. Anderson cite barriers that remain in successfully achieving the patient outcomes (including satisfaction) and reducing cost.
“Health plans have been unable to successfully deal with many complex patients,” says Dr. Anderson, noting that plans often do not spend enough resources on getting the program in place, as well as not identifying patients who most likely will benefit from their program.
Dr. McCarthy also points to the lack of supportive financial incentives for programs that still have fee-for-service reimbursement arrangements, as well as the challenge of developing the capacity to make changes in practice (including training and new skills to take on new roles), putting a data infrastructure in place to share information among care team members in a timely way, and scaling up evidence from research pilot projects and trials to what will work in everyday practice.
Overall, Dr. McCarthy emphasizes keeping the focus on the patient when developing and implementing a program with an eye to improving patient outcomes and reducing cost.
Key Message for Providers
For rheumatologists and other providers who see patients with multiple chronic conditions, Dr. Anderson emphasizes the need to include someone who coordinates all of the care of each patient. “The care coordinator needs to look at the patient’s entire medical situation, their social needs and their economic situation to help them make the proper decisions,” he says, adding that rheumatologists need to address more than the rheumatologic concerns of these patients to provide sufficient care.
Dr. McCarthy also highlights the need to keep the needs and wants of the patient front and center. “Know your patients and redesign your systems and routines to meet their needs,” he says, adding that colleagues at the Institute for Healthcare Improvement recommend getting help from patients. “Enlist the help of five patients by asking them and their family members to share their experiences with healthcare,” he says, asking such questions as, “Where are they encountering frustrations? How can you improve the ways they get care and help them realize their goals for care?”
