The Case
A 64-year-old previously healthy man was admitted to the hospital with a 1.5-month history of severe headache, confusion, personality change, and progressive cognitive decline. He had no previous medical problems. Results of the physical examination showed ataxia. The mental status exam revealed impairment of cognitive functions. Laboratory test findings were unremarkable. The erythrocyte sedimentation rate was 2 mm/hour. Tests with normal or negative findings included serum antinuclear antibodies, antineutrophil cytoplasmic antibodies, antibodies against double-stranded DNA, cryoglobulins, anticardiolipin antibodies, blood coagulation studies, tuberculin skin test, serology tests (for hepatitis B, hepatitis C, and human immunodeficiency virus), and a fungal serology survey (Coccidioides, Histoplasma, and Blastomyces). Cerebrospinal fluid (CSF) protein concentration was 97 mg/dl (normal, 14–45 mg/dl), erythrocyte cell count was 50/ul, and white blood cell count was 23/ul (90% lymphocytes, 10% monocytes). Cytologic findings were normal. Additional CSF tests with negative results included the venereal disease research laboratory test, Cryptococcus antigen test, fungal and bacterial cultures, and polymerase chain reaction assays for herpes simplex and zoster viruses, Epstein-Barr virus, cytomegalovirus, Toxoplasma gondii, and Borrelia burgdorferi.
Findings on a chest radiograph, transesophageal echocardiogram, and duplex carotid ultrasonogram were unremarkable. Initial contrast-enhanced magnetic resonance imaging (MRI) of the brain showed diffuse bilateral leptomeningeal enhancement involving the cerebrum and the cerebellum, multiple infarcts, and patchy T2-weighted white matter signal abnormality. Conventional cerebral angiography was normal.
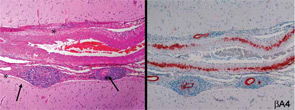
Because of the clinical history and MRI findings, a diagnosis of primary central nervous system vasculitis (PCNSV) was considered, and an open brain biopsy was performed. Pathology showed granulomatous leptomeningeal and intraparenchymal vasculitis. Infarcts and vascular beta-A4 amyloid deposition consistent with cerebral amyloid angiopathy (CAA) were also present (see Figure 1). Stains of biopsy specimens were negative for fungal and mycobacterial organisms.
PCNSV associated with CAA was diagnosed, and the patient was treated with oral prednisone (initial dosage, 40 mg/day) and monthly pulse intravenous injections of cyclophosphamide (CYC) (1.7 gm/month) for 14 months. The patient’s neurologic state progressively improved in the first three months. He was much less confused, his headache resolved, and he was able to perform many of his previous activities. At the time of follow-up, cranial MRI showed complete resolution of leptomeningeal enhancement and no new infarcts. At his final visit 12 months later, the patient was no longer receiving prednisone or immunosuppressives and had no recurrence of symptoms attributable to vasculitis. He had only a minimal disability and conducted normal activities.
PCNSV
PCNSV is a poorly understood form of vasculitis that is limited to the brain and spinal cord and occurs in both adults and children.1,2 PCNSV represents the most frequent form of vasculitis involving the CNS (see Table 1).3 Modern recognition of PCNSV as a separate entity is generally dated to the mid-1950s when Cravioto and Feigin described several cases with a “non-infectious granulomatous angiitis” with a predilection for the nervous system.4 PCNSV is a rare condition. The only reported incidence rate estimate for PCNSV derives from Olmsted County, Minn., and is 2.4 cases per 1,000,000 person-years. Men and women are similarly affected. The median age at diagnosis is approximately 50 years.1


