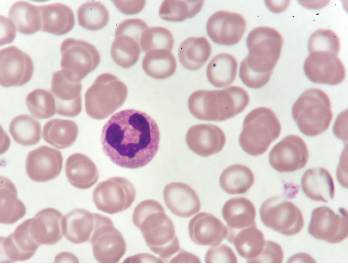
A neutrophil in a blood smear.
Jarun Ontakrai / shutterstock.com
Certain medications have been associated for decades with the development of drug-induced autoimmunity. New research published in March 2018 in Arthritis & Rheumatology suggests that NETs (neutrophil extracellular traps) are potentially implicated in the mechanisms that lead to drug-induced autoimmunity.1
Peter Grayson, MD, MSc, head of the Vasculitis Translational Research Program at the National Institute of Arthritis and Musculoskeletal and Skin Diseases, says that research related to NETs may have no current clinical implications, but he predicts that research focused on NETs “is likely to unlock novel therapeutic strategies in a range of rheumatologic diseases.” Understanding the role of NETs in drug-induced autoimmunity may be the next step toward clarifying the mechanisms of autoimmunity.
NET formation is involved in the neutrophil cell death process, called NETosis, which is different morphologically from other types of cell death, including apoptosis and necrosis. In NETosis, the dying neutrophils “can unwind their DNA and launch it out of the cell like a spiderweb to engulf and facilitate the elimination of pathogens,” Dr. Grayson explains. The process, however, can become aberrant in many rheumatologic diseases with the dysregulation of NET formation.
“What is surprising and potentially interesting for rheumatologists to understand is that there is only a small number of proteins inside these NETs, and many of them are the antigenic targets of autoantibodies in rheumatologic diseases,” Dr. Grayson says. Patients with rheumatoid arthritis make anticyclic citrullinated peptide (CCP) antibodies directed to proteins found in the NETs. Patients with lupus make antibodies to NET components. Proteinase 3 and myeloperoxidase, the antigenic targets of antineutrophil cytoplasmic antibodies (ANCA) are commonly found within NETs.
“These proteins that are normally hidden inside a neutrophil get exposed to the adaptive immune system in a way that is immunogenic, which then can potentially lead to development of antibodies to those proteins,” says Dr. Grayson.
NET formation and impaired NET degradation have been implicated in the pathogenesis of both systemic lupus erythematosus (SLE) and ANCA-associated vasculitis (AAV). “The process of NETosis may contribute to causal mechanisms of disease in rheumatoid arthritis, lupus and AAV,” he says.
In NETosis, the dying neutrophils ‘can unwind their DNA & launch it out of the cell like a spiderweb to engulf & facilitate the elimination of pathogens,’ Dr. Grayson explains.
Triggering NET Formation, Degradation
Previous research that examined drug-induced autoimmunity looked at the effect of medications on lymphocytes. This new research by Dr. Grayson and colleagues looked at their effect on neutrophils and NETs. Medications associated with drug-induced autoimmunity can lead to development of a rheumatologic disease that “has a specific look or feel to it. It looks a lot like lupus mixed with ANCA vasculitis. We thought that because NETs are important in lupus and ANCA vasculitis, maybe the drugs are inducing NETs, since it’s a common theme to those conditions,” Dr. Grayson explains.


