In snapping triceps, with elbow flexion of approximately 115º, the distal MHTr also dislocates over the apex of the medial epicondyle, with or without audible/palpable snapping, and may push the ulnar nerve out of the groove (subluxation), perhaps to a point over the apex of the medial epicondyle (dislocation).1,3,4 Hypertrophy of the triceps may be a predisposing condition to ulnar nerve dislocation.1
Tommy John Surgery
Orthopedic surgeon Frank Jobe first performed ulnar collateral ligament (also called the MCL) reconstruction on baseball pitcher Tommy John in 1974.5 The procedure was named for the first recipient.
In this procedure, a soft tissue graft, most commonly a palmaris longus or gracilis autograft, is used as a functional substitute for the anterior bundle of the ulnar collateral ligament complex. The ulnar nerve may or may not be transposed as a part of this procedure, based on the patient’s history, physical exam findings, imaging studies and surgeon preference in consultation with the patient.
Most patients do well, with good to excellent results and a high rate of return to play after this surgery, but complications do occur.6 The average complication rate is 10.2%, with the majority (6.7%) of complications being ulnar nerve neurapraxia.6
Since Dr. Jobe performed the first Tommy John surgery in 1974, the incidence of this procedure has risen dramatically. In a recent study looking at the prevalence of medial ulnar collateral ligament surgery in 6,135 current professional baseball players, 13% of all Major and Minor League Baseball players and an astonishing 20% of Major and Minor League pitchers have undergone Tommy John surgery.7
What about the MCL in asymptomatic professional baseball pitchers? There is a substantial incidence of MCL abnormalities on MRI in asymptomatic professional baseball pitchers. Two studies revealed a 15% and a 27% incidence of asymptomatic MCL tears in this population.8,9
Out of the Ulnar Groove
Since at least 1896, physicians have known the ulnar nerve may move out of the ulnar sulcus in elbow flexion; however, the clinical ramifications have been better understood only in the past few decades.10 The term ulnar nerve instability was described in 1977. This occurs when the ulnar nerve chronically subluxes and relocates with elbow flexion and extension.11 This increases ulnar nerve vulnerability to trauma, particularly when it lies superficially on the medial epicondyle.12 The most common probable cause of ulnar nerve instability is ligamentous laxity.12
Hypertrophy of the MHTr acquired from exercise is also postulated to be a cause of ulnar nerve instability and snapping triceps syndrome.1,13,14 Ulnar nerve instability may occur with or without radiating paresthesia and with or without snapping of either the ulnar nerve or the MHTr.12,15 It is a separate entity from ulnar nerve compression, although a friction neuritis may produce radiating paresthesia mimicking cubital tunnel syndrome.12
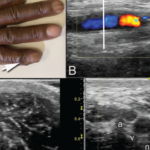
Snapping elbow is undetected by standard (static) radiographs and MRI.3 Thus, dynamic ultrasonography is becoming the gold standard when evaluating medial elbow pain occurring with movement.3,4 Prior to the use of dynamic ultrasonography, nonroutine, flexion and extension MRI views were required to image a snapping triceps.4,5,16 Dynamic ultrasonography is inexpensive and simple to perform at the point of care.
Discussion
In our patient, the history, physical examination and dynamic sonographic study did not reveal snapping of either the ulnar nerve or the MHTr during elbow flexion. The patient, therefore, did not suffer from classic snapping elbow, either snapping ulnar nerve or snapping triceps muscle. Pain occurred only at the end of rapid and forceful full elbow extension, that is, the motion utilized when throwing a baseball. Because the dislocated ulnar nerve did not produce paresthesia, either with dislocation or forceful relocation, electrophysiological studies were not determined to be necessary.
Static ultrasonography done during elbow extension verified the ulnar nerve to be in its proper position in the ulnar groove. Dynamic ultrasonography revealed the ulnar nerve to completely dislocate out of the ulnar groove during elbow flexion, being propelled over the medial epicondyle by the hypertrophied MHTr. Vigorous relocation of the ulnar nerve upon rapid elbow extension was the source of localized medial elbow pain. Complete resolution of the pain occurred after ulnar nerve transposition. The MHTr muscle was left intact during surgery and was not the source of medial elbow pain.
We describe this as ulnar nerve relocation pain, and we propose characterizing this as a syndrome. The elements of this proposed syndrome would be: sonographic demonstration of ulnar nerve dislocation pushed by a hypertrophied and dislocating MHTr muscle, with pain occurring at the end of rapid elbow extension. The typical clinical setting would be in a professional athlete who repetitively throws.
In patients with medial elbow pain and particularly in those with pain occurring after MCL reconstruction procedure, it may be reasonable to perform an ultrasonography exam, including a dynamic exam to evaluate for a cause not apparent on an MRI.
Further, given the substantial incidence of asymptomatic, incidental MCL tears on MRI in professional baseball pitchers, consideration of ulnar nerve relocation syndrome may help avoid unnecessary MCL reconstruction surgery or prompt consideration of concomitant ulnar nerve transposition, if such surgery is deemed necessary.
 Mark H. Greenberg, MD, RMSK, RhMSUS, is board certified in internal medicine and rheumatology. He is an associate professor of medicine at the University of South Carolina School of Medicine at Prisma Health USC Medical Group, Columbia, S.C.
Mark H. Greenberg, MD, RMSK, RhMSUS, is board certified in internal medicine and rheumatology. He is an associate professor of medicine at the University of South Carolina School of Medicine at Prisma Health USC Medical Group, Columbia, S.C.
 A. Lee Day, MD, RMSK, is board certified in internal medicine and rheumatology. He is a rheumatologist at Prisma Health USC Medical Group, Columbia, S.C., and is an assistant professor of internal medicine at the University of South Carolina School of Medicine.
A. Lee Day, MD, RMSK, is board certified in internal medicine and rheumatology. He is a rheumatologist at Prisma Health USC Medical Group, Columbia, S.C., and is an assistant professor of internal medicine at the University of South Carolina School of Medicine.
 James W. Fant Jr., MD, is board certified in internal medicine and rheumatology. He is an associate professor of medicine at the University of South Carolina School of Medicine and director of the Rheumatology Division at Prisma Health USC Medical Group, Columbia, S.C.
James W. Fant Jr., MD, is board certified in internal medicine and rheumatology. He is an associate professor of medicine at the University of South Carolina School of Medicine and director of the Rheumatology Division at Prisma Health USC Medical Group, Columbia, S.C.
 Christopher G. Mazoue, MD, completed a sports medicine fellowship at the American Sports Medicine Institute. He is an associate professor and chair of the USC Department of Orthopedic Surgery and the Prisma Health USC Orthopedic Center, and medical director for the USC Gamecocks athletes.
Christopher G. Mazoue, MD, completed a sports medicine fellowship at the American Sports Medicine Institute. He is an associate professor and chair of the USC Department of Orthopedic Surgery and the Prisma Health USC Orthopedic Center, and medical director for the USC Gamecocks athletes.