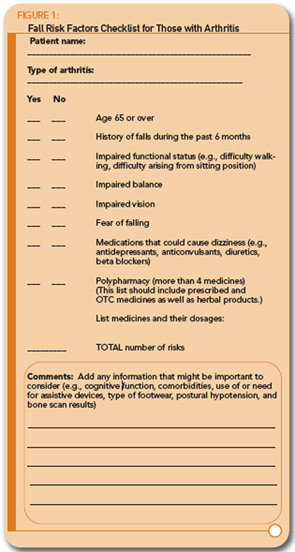
Both polypharmacy (i.e., taking more than four medicines) and dizziness have been identified as common fall risk factors. A review of medicines the person is taking, including over-the-counter (OTC) medicines and herbal preparations, thus, becomes an important part of the assessment. Because dizziness is one of the risk factors, medicines that could possibly cause dizziness should be discussed with the patient to determine if this could be a contributing factor. Dizziness as a possible side effect should be discussed, as appropriate, when a new medicine is started. Antidepressants are commonly cited as a problem because they can lower blood pressure, resulting in dizziness. Some of the other drugs that may be an issue include diuretics, beta blockers, and anticonvulsants. It is not unusual for individuals to have several chronic conditions and take a number of different medications, especially as they age. Taking more than four medicines may signal that a reevaluation of drug therapy is needed. Factors important to consider include whether a different medicine might be more appropriate; whether the medicine dosage might be reduced, noting that older individuals generally need a smaller amount; when the medicine should be taken to lessen dizziness-related issues, and whether there are possible interactions that are causing harm.
Numerous other factors deserve consideration on an individual basis, including cognitive function, number and type of comorbidities, use of or need for assistive devices, and type of footwear. An additional test that importantly and indirectly relates to assessment for fall prevention is a bone density scan. Individuals with low bone mass are at higher risk for injury due to fracture when they fall. Any person who experiences a number of osteoporosis risk factors9 should be evaluated with a dual-energy X-ray absorptiometry, or DXA. It is important that those with validated low bone mass and high fracture risk be carefully evaluated for possible fall risks.
Intervention: Assessment follow-up depends on the individual findings. If individuals show that they do have fall-related risks, they should be referred to a comprehensive falls prevention program, if available, or to appropriate healthcare professionals. Much of the needed follow-up can be provided in the office, clinic, or home settings by a nurse or nurse practitioner and a physical therapist working in collaboration with the physician. Two components of a fall prevention program are needed and can be addressed in either setting; these include (1) discussion and education and (2) exercise and training.6,20 Involving individuals in their own preventive treatment is important for reducing their own falls, and fall risks will be largely dependent on adherence to prescribed activities.