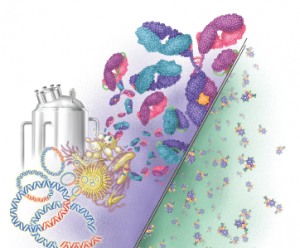
Right: The small molecule structure of aspirin (21 molecules). Left: A monoclonal antibody made up of 10,000–20,000 molecules.
DNA Illustrations / Science Source
As questions about biosimilar medications swirl among U.S. rheumatologists, a recently released report sheds some light on the European experience with biosimilars—and may offer some important insights for the U.S. market.
The report, Biosimilars in the EU: Information Guide for Healthcare Professionals, was released in late April by the European Medicines Agency (EMA) and the European Commission.1 Highlights:
- Biosimilars have been in the European Union (EU) since 2006, and the EU has approved the highest number of biosimilars worldwide.
- The EU monitoring system for safety concerns has not identified any relevant difference in the nature, severity or frequency of adverse effects between biosimilars and their reference medicines since their approval.
- Although biosimilars may have minor differences from their reference medicines, these differences are not clinically meaningful. There are no expected differences in safety and efficacy.
- Biosimilars in the EU have been approved using the same standards of pharmaceutical quality, safety and efficacy as those of all biological medicines.
- A biosimilar can rely on the safety and efficacy gained during research with the reference medicine. This means clinical trials are not needed for each indication for which the biosimilar seeks approval.
- Because an approved biosimilar is very similar to its reference medicine and has the expected comparable safety and efficacy in one therapeutic indication, data can be extrapolated to other indications for which the reference medicine has been approved. “Extrapolation needs to be supported by all the scientific evidence generated in comparability studies,” according to the report.
- Biosimilar competition offers benefits to EU healthcare systems because it can improve patient access to safe and effective medicines with proved quality.
The findings from the report demonstrate Europe’s 10-year head start compared with the U.S. market, says Angus B. Worthing, MD, FACP, FACR, Arthritis & Rheumatism Associates, in the Washington, D.C., area, and chair of the ACR’s Government Affairs Committee. “Biosimilars were first approved in Europe more than 10 years ago and with more than 25 drugs in use, none has been pulled for safety problems. Pharmacovigilance programs have not identified any safety issues in biosimilars that differed from reference drugs,” he says.
This broad experience contrasts with that in the U.S., which has just six biosimilars approved by the U.S. Food and Drug Administration (FDA) (see Table 1).



