Many of us initially saw these persistent performance gaps as either our own individual failure or as a failure on the part of our patients to keep scheduled appointments. To systems analysts, however, these persisting gaps instead suggest a classic systems capacity bottleneck in which available resources (in this case visit slots) are too few to allow timely performance of required work (in this case disease activity assessments) at the recommended intervals.7 This visit capacity bottleneck causes a stalemate wherein the number of patients reassessed each month is equal to the number that become overdue. In any business, meeting basic customer needs is fundamental to success; our registry data suggest that we are not achieving this standard in our RA management.
Population management enables clinicians to provide timely disease activity measurement & recommended care.
This problem was confirmed by more detailed capacity analyses of 20 RAPP Project practices (see Figure 2, for an example). The magnitude of the visit capacity bottleneck among these practices is influenced by RA population numbers, days practiced per month, numbers of patients scheduled per day, percentage of visits allocated to managing established RA patients, and finally distribution of disease activity in the disease population. When physicians schedule additional out-of-office activities, our capacity bottleneck worsens. Simply put, this bottleneck compromises our RA disease assessments and management—and we were all blind to the problem until we analyzed the data from our population management registries.
(Click for larger image)
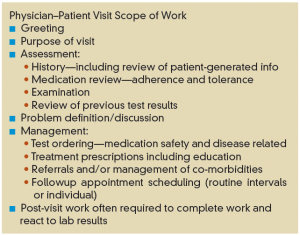
Figure 3: Typical scope of work associated with an RA established patient visit.
The evidence for time constraints during individual visits is equally sobering. The time scheduled, typically 20 minutes, is generally insufficient for the physician to perform all the necessary work (see Figure 3). The infrequent use of composite disease activity assessments by RAPP physicians and other rheumatologists is due at least in part to the lack of time available to perform them.5 However, scheduling longer visits just worsens the bottleneck, and, too often, an urgent patient need trumps the intended disease assessment and management.
The Visit Capacity Bottleneck Is a System-Design Problem
Once RAPP clinicians realized that working harder wouldn’t help close our care gaps, we were faced with four seemingly stark options: 1) accept our current performance as being the best we can do; 2) severely reduce our patient panel sizes to fit available provider appointment slots; 3) add additional rheumatologists to our practices; or 4) change how we assess RA disease activity and who does it.

