(click for larger image)
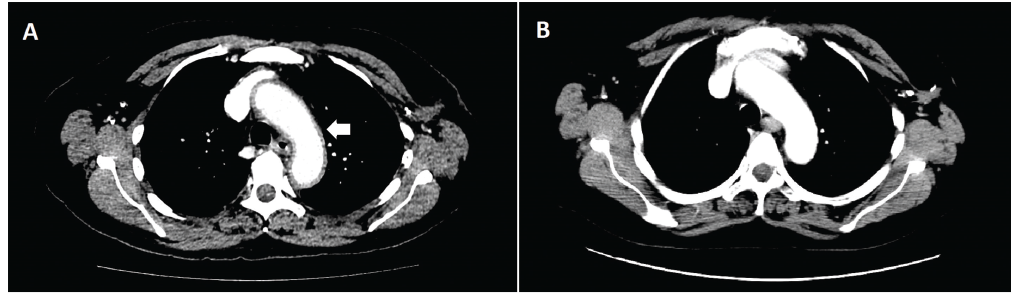
Figure 1: An axial CT image of the chest revealed diffuse aortic wall thickening and periaortic inflammation involving the thoracic aorta, origins of neck vessels, and abdominal aorta consistent with aortitis at time of presentation (Panel A). Inflammation involving the aortic arch can be seen here (white arrow). A follow-up CT one month later (Panel B) reveals near-complete resolution of aortitis after systemic corticosteroid therapy.
Within days of initiation of treatment with steroids, she experienced significant improvement in her symptoms and was discharged home with prednisone 60 mg by mouth daily. Outpatient rheumatology referral was then requested.
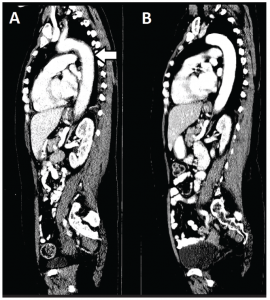
At the time of her initial outpatient appointment, the patient had been treated with prednisone 60 mg daily for one week and then tapered to 50 mg daily by oncology for one month. A repeat CT of the chest, abdomen and pelvis at this time point revealed near-complete resolution of the soft tissue diffuse wall thickening of the thoracic aorta, with only minimal thickening at the aortic arch. There was also resolution of the lower lobe patchy airspace opacities, pleural effusions and pericardial effusion.
The plan was to taper the prednisone by 10 mg every two weeks to a dose of 20 mg daily. However, the patient self-tapered her prednisone and discontinued the prednisone after another four weeks.
Two weeks after she stopped her prednisone taper, she experienced a recurrence of her previous symptoms and was promptly placed back on prednisone 20 mg daily. Currently, she is undergoing a slower taper of prednisone, and her symptoms are well controlled. If she experiences recurrent symptoms, the plan would be to treat with infliximab, given reports of successful treatment of other irAEs with this drug.
Prolonged steroid taper may be necessary with severe immune reactions & mirrors our treatment of other large vessel vasculitis with regard to prednisone dosing.
Discussion
(click for larger image)
Figure 2: A sagittal CT image of the chest, abdomen and pelvis reveals the extent of aortitis (white arrow) at time of presentation (Panel A) and one month later with systemic corticosteroid therapy (Panel B).
Immune-checkpoint-blocking antibodies have been successful in treating advanced melanoma. The FDA has approved four immune checkpoint inhibitors: ipilimumab (anti-CTLA-4), nivolumab [anti-programmed cell death protein 1 (anti-PD-1)], pembrolizumab [anti-programmed death-
ligand 1 (anti-PD-L1)] and atezolizumab (anti-PD-L1).3 However, enhancement of the immune response against tumors can also induce a wide spectrum of irAEs that may require discontinuation of therapy.