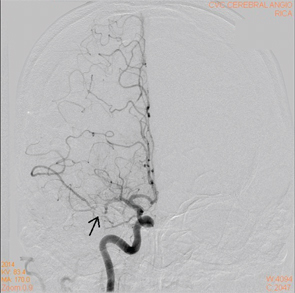
Figure 5A: A cerebral angiogram showing right MCA stenosis.
Compared with PACNS, CSF analysis is usually unremarkable in patients with moyamoya disease; however, unlike PACNS, diagnosis of moyamoya is typically made on the basis of radiological findings.7 To diagnose moyamoya disease, the following MRI–MRA criteria need to be met:5,6
- Stenosis or occlusion of the terminal part of the ICA and/or the proximal portion of the ACA and/or MCA;
- Visualization of an abnormal arterial vascular network around the stenotic and/or occluded lesions; and
- Symmetry of the lesions, showing bilateral involvement.
Therefore, conventional digital subtraction angiography remains the gold standard for diagnosing moyamoya disease.7
Because of moyamoya disease’s ability to mimic central nervous system vasculitis, it is important for rheumatologists to recognize this condition & diagnose it appropriately.
Treatment
Because PACNS is a very rare disease, no good randomized control trials comparing one treatment modality with another exist. The most commonly accepted treatment typically consists of glucocorticoids, possibly with cyclophosphomide.1
For moyamoya disease, no evidence suggests any benefit from corticosteroid therapy. Surgical revascularization for patients with ischemic moyamoya disease has been shown to decrease the frequency of transient ischemic attacks and risk of cerebral infarction.
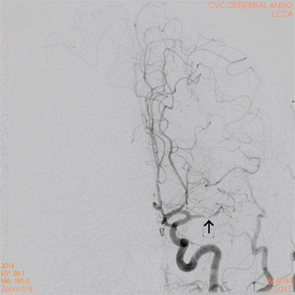
Figure 5B: A cerebral angiogram showing left MCA stenosis.
On the other hand, for patients who cannot undergo surgical intervention, either due to recent infarction or good spontaneous revascularization, medical therapy with a cerebroprotective agent, edaravone, and an antithrombotic agent, such as aspirin, ozagrel, argatroban or heparin, is recommended. For hemorrhagic moyamoya disease, ventricular drainage and hematoma evacuation are the treatment modalities of choice.6
Conclusion
On initial presentation, both PACNS and moyamoya disease present similarly. Because treatment differs significantly, it’s important to differentiate between the two disorders. Given that both disorders can lead to permanent, serious, neurologic damage, it’s crucial that an accurate diagnosis be made so the correct treatment can be initiated as soon as possible.
Unlike PACNS, diagnosis of moyamoya is typically made on the basis of radiological findings.
Hopefully, by continuing to learn of these new cases, physicians will be better equipped to diagnose and treat these disorders appropriately and, thus, improve patient outcomes.
Dr. Kim
Joey Kim, MD, is an internal medicine resident currently finishing his third year of residency at Stony Brook University Hospital in New York. He hopes to pursue a career in rheumatology in the future.
Megha Patel-Banker, MD, is a board-certified rheumatologist who completed her fellowship training at Stony Brook University Hospital and currently practices in the Dallas area.