Pikoso.kz / shutterstock.com
I nodded, gravely.
I was recently privileged to attend a symposium on eosinophils. I realize that this sounds odd. And it was odd, mainly because I’m not an eosinophil expert. Still, they were in need of someone who knew something about eosinophilic granulomatosis with polyangiitis, so I managed to sneak in through the back door.
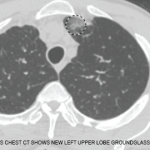
As an aside, I think we are on the cusp of a revolution in how we think about diseases mediated by eosinophils. Although we treat them as distinct diagnoses, a tremendous amount of clinical overlap exists between eosinophilic granulomatosis with polyangiitis and other diseases mediated by eosinophils (e.g., chronic eosinophilic pneumonia, eosinophilic esophagitis and other idiopathic hypereosinophilic syndromes). Interestingly, all of these syndromes seem to respond to therapy directed against interleukin 5, regardless of what you call them. Eventually, mepolizumab, reslizumab, benralizumab and other such drugs may unify these diagnoses, in the same way that rituximab has brought together idiopathic orbital pseudotumor, Mikulicz syndrome and idiopathic pancreatitis under the rubric of the IgG4-related diseases.
We are still at just the early stages, however, of understanding diseases mediated by hypereosinophilia. Because of this, at this symposium, we were given a task: propose what we would need to make a breakthrough. Unlike in most grant brainstorming sessions, we were specifically instructed not to consider the cost.
As you could imagine, our proposal quickly spiraled from unlikely to ludicrous. First, we needed substrate: knowing the environment can stimulate eosinophils, we proposed collecting samples from all continents, from patients at all decades of life. We then had to figure out how to characterize these samples. After some back and forth, one of the PhDs in the group exclaimed, “Drop-seq!”
I nodded, gravely.
I was nodding to disguise the fact that I had no idea what he was talking about.
Recently, I’ve been doing a lot of that sort of grave nodding. Seq in these cases stands for sequencing, and the suffix seems to be making its way into a lot of conversations. I know that techniques like PhIP-seq and Drop-seq have dramatically sped the process of discovery. But what do they mean?
Autoantibody Discovery
Let me know when the antibodies come back. As a consultant, I have spoken these words hundreds of times. Autoantibodies are so central to how we think about rheumatic disease, both in terms of classification and pathogenesis, that I am generally loathe to make a final diagnosis if that information is not yet firmly in hand. But how did we come to identify these autoantibodies in the first place?
Consider, for example, mixed connective tissue disease. Undifferentiated connective tissue disease is the catchall label we give patients we suspect have some autoimmune phenomenon that has not yet been given a proper name. Mixed connective tissue disease was first described by Sharp et al. in 1972, when he identified 25 patients who had features of systemic lupus erythematosus, scleroderma and polymyositis.1 Sharp noted these patients were unified by the presence of antibodies against ribonucleic protein (RNP). He described the process of identifying the presence of these anti-RNP antibodies thus:
To study the specificity of antibodies … enzymatic digestion studies were performed. Treatment of the ENA antigen on the red cells with RNase completely eliminated or markedly reduced the agglutination reaction with the patient’s serum in every case of mixed connective tissue disease whereas treatment with trypsin reduced the titer to some extent. Treatment with DNase had no effect. … [T]he speckled pattern of the antinuclear fluorescence was eliminated by treatment of tissue sections with RNase but not DNase prior to incubating them with serum from patients with mixed connective tissue disease.
In other words, they conducted a series of experiments to narrow the biochemical properties of the autoantigen. But they also got lucky: The autoantigen just happened to be something that could be affected meaningfully by the reagents they had available.
This observation is not meant, by any means, to denigrate the value of their work. Happenstance is often a valuable partner in discovery. There is no particular reason, for example, that antibodies that recognize proteins in the cytoplasm of neutrophils should be associated with glomerulonephritis, but the discovery of anti-neutrophil cytoplasmic antibodies (ANCA) must be one of the most important advances made in our understanding of the systemic vasculitides.2 Similarly, a breakthrough in our understanding of immune-mediated necrotizing myopathies came from the recognition that autoantibodies from some of these patients bound to a protein that was the same molecular weight as 3-hydroxy-3-methylglutaryl coenzyme A reductase (HMGCR), an enzyme better known to you as the pharmacologic target of statins.3
The right insight, with the right reagent, at the right time. These are the classic ingredients for autoantibody discovery. And with these ingredients alone we would undoubtedly continue to lurch toward discovery, occasionally achieving new insights, interspersed with long periods of frustrating silence.
Identifying the presence of a specific autoantibody when you have a specific target in mind is not difficult: an autoantibody target (generally, a protein) is bound to the bottom of a plate. Serum from the patient is introduced, and you see if the patient has an antibody that binds to the target. This, in a nutshell, is how the enzyme-linked immunosorbent assay (ELISA) works and is the foundation of the diagnostic antibody testing that keeps Quest Diagnostics and LabCorp in business.
Identifying a novel autoantibody when you don’t know what the target might be is more difficult. If you were using ELISA, you could methodically work your way through every target, one by one. Of course, empires would rise and fall in the time it would take to search through the more than 20,000 proteins manufactured by the human genome.4
Enter PhIP-seq.
One advance in autoantibody discovery came through the use of viruses known as bacteriophages. A phage-display library incorporates human DNA into the viral genome, allowing various human peptides to become part of the viral coat.5 Picture a football stadium in which all the fans were asked to hold banners high over their heads so the cameras could get a good look at each sign. Now, instead of banners, picture every fan holding a small protein fragment; instead of a camera, picture an antibody searching for its target. This is basically how a phage display library works.
The problem with this technique is that not every bit of DNA will be correctly incorporated by the viral genome. Therefore, the proteins expressed by the viruses often represent an incomplete version of reality. Even under the best of circumstances viruses can display only fragments of proteins, not complete proteins with their tertiary structures intact. It’s like reading a sonnet when not every word is successfully printed on the page—you may still see enough to get the gist, or you may just completely miss the point.
Phage immunoprecipitation sequencing (PhIP-seq) uses viruses to display the peptidome: a close-to-complete set of protein fragments encoded by the human genome.6 Because the peptidome uses protein fragments and not complete proteins, not every human autoantibody will be able to find an appropriate target, even with this system. But it allows us to get much closer to this goal than was previously possible.
Of course, this one sentence belies the tremendous complexity of the work that follows: Once an antibody binds a protein, the antecedent DNA must be amplified, then sequenced, to identify the target. But it is not hard to see how this technique could open doors previously slammed shut.