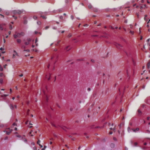
joel bubble ben / shutterstock.com
In a controlled, large-cohort, longitudinal study from Canada, Atiquazzaman et al. found that use of non-steroidal anti-inflammatory drugs (NSAIDs) substantially contributes to increased cardiovascular disease risk among people with osteoarthritis (OA).1
This is the first study to evaluate the mediating role that NSAIDs play in the association between OA and cardiovascular disease (CVD), and the findings show that a significant percentage of the effect of OA on heart disease risk is mediated through NSAIDs.
Although research shows OA is an independent risk factor for cardiovascular disease, “what we didn’t know was why,” says Aslam H. Anis, PhD, FCAHS, professor, School of Population and Public Health, University of British Columbia, Vancouver, and a co-author on the study.2
“The research gap was understanding the mechanism of the increased risk of CVD among OA patients compared to the general population. People with OA are frequently treated with NSAIDs to control their pain and inflammation, and it’s well known that NSAIDs are associated with cardiovascular adverse effects,” Prof. Anis says.
Many studies also link NSAID use to an increased risk of heart-related events: One 2008 cohort study of 336,906 individuals found that stroke risk was 20% higher for those who used indomethacin and 28% higher for those who used rofecoxib.3 In contemplating these interrelationships, Prof. Anis and his colleagues wanted to investigate the role of NSAIDs in the observed association between OA and CVD, and to better understand the relationship.
Mediating Effect
Atiquazzaman et al. analyzed health administration data from a population-based cohort of 720,055 individuals in British Columbia. They identified 7,743 OA patients matched on age and sex, as well as 23,299 patients who did not have OA as controls. The study’s primary outcome was the risk of developing incident CVD, and the secondary outcomes were the risk of developing ischemic heart disease, congestive heart failure and stroke. Their focus was estimating the mediating effect of NSAIDs, which they defined as current NSAID use, on the relationship between OA and CVD.
Based on population-based health administration data from British Columbia’s healthcare system, Atiquazzaman et al. found that people with OA had a 23% higher risk of developing CVD than those without OA. This finding was in line with the results of previous studies, including a 2016 meta-analysis of 15 different observational studies that found a 24% higher risk of CVD among OA patients compared with healthy individuals.4