The study also highlights the current and future maldistribution of adult rheumatologists practicing in the U.S., with 21% of rheumatologists in the Northeast compared with only 3.9% in the Southwest. “In 2015, the ratio of provider per 100,000 patients by region ranged from 3.07 in the Northeast to 1.28 in the Southwest,” note the authors. “By 2025, there is an anticipated decrease in all regions, ranging from 1.61 in the Northeast to 0.50 in the Northwest.”
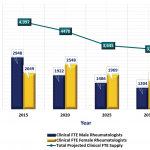
In their discussion, the authors note the need for creative solutions. “These results represent a dramatic decline in the rheumatology workforce from 2015 to 2030,” they write. The authors also suggest potential strategies to address some of these workforce challenges, including recruiting nonphysician providers, encouraging changes in the regional distribution of the workforce, expanding telemedicine programs, retaining international medical graduates who train in rheumatology and improving practice efficiencies.
In response to the 2005 workforce study, the number of first-year adult fellowship training positions increased from 156 to 210, with over 95% fill-rate each year. To leverage the potential for positive change in wake of the 2015 study, authors note that creative strategies for the retention of international medical graduates and new entrants into the rheumatology workforce are warranted.
The authors also highlight how financial incentive programs, which offer scholarships, loans with service requirements and loan repayment or forgiveness, may aid rheumatology. They write, “Expanding financial incentives with service requirements may increase access to care in rural and underserved communities. Surveys suggest that competitive salaries, professional development, knowledgeable support staff and professional support increase the likelihood of provider retention in rural or underserved areas after completion of service commitments.”
The authors also note that since the 2005 study, “nurse practitioners and physician assistants have been shown to be quite effective in managing treat-to-target goals in a rheumatology practice.” They encourage the further exploration into recruitment and training strategies that enable nurse practitioners and physician assistants to be included into the adult rheumatology workforce.
“The ACR/ARHP is committed to optimizing quality rheumatology care and facilitating access to rheumatology care,” conclude the authors. “This will require a passionate vision and innovative strategies by the ACR/ARHP, as well as at the state and federal levels … Decreasing insurance barriers and healthcare regulations may allow more rapid, timely, and creative solutions to offset the projected rheumatologist shortage and the maldistribution of rheumatologists in the U.S.”