(Click for larger image)
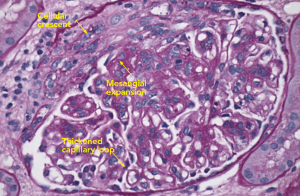
Figure 2: PAS Staining
Example of a glomerulus that contains a focal cellular crescent and expanded mesangium. Thickened capillary loops suggest double contouring of the basement membrane (see Electron Microscopy, Figure 4).
Due to her history of SLE, elevated blood pressure and new-onset nephrotic range proteinuria, the nephrology service performed a kidney biopsy early in her admission to determine if she had developed lupus nephritis. Light microscopy of the kidney biopsy revealed multiple glomeruli containing mesangial expansion and cellular crescents (see Figure 1). Immunofluorescence staining demonstrated faint, granular deposits of IgG and IgM across glomeruli, and C3 along capillary walls (see Figure 2).
In general, lupus nephritis kidney biopsies can exhibit mesangial expansion and cellular crescents, along with strong immunofluorescence staining for IgG, IgM, IgA, C3, C1q, which is known as a “full house.” In this case, the presence of faint granular immunofluorescence and cellular crescents suggested another diagnosis, like ANCA-associated pauci-immune kidney vasculitis.
Approximately 15–20% of SLE patients test positive for ANCA, although the clinical significance is not clear.1 Some data suggest that positive ANCA testing in lupus patients is associated with nephritis or an overlap syndrome, consisting of lupus nephritis and pauci-immune crescentic glomerulonephritis, which is rare and found in case reports.2 In this patient, the initial biopsy findings suggested an ANCA-associated pauci-immune kidney vasculitis, so she was empirically treated as such. For induction, she received intravenous methylprednisolone 1 g for three days, followed by weight-based oral prednisone of 1 mg/kg. Rituximab (375 mg/m2) was administered, and to be given once weekly for four weeks. Using rituximab in this clinical setting was based on clinical trial data comparing rituximab with cyclophosphamide treatment in patients with newly diagnosed ANCA-associated kidney vasculitis (but without SLE). There was no difference in relapse, death or end-stage kidney disease at two years.3 She was discharged with a steroid taper and outpatient visits to receive rituximab.
Several days after discharge, new diagnostic information returned. Electron microscopy of the kidney biopsy revealed large subendothelial deposits with adjacent substructures and serum cryoglobulins returned at 4% (normal negative), suggesting that her initial presentation was due to cryoglobulinemia, rather than ANCA-associated pauci-immune glomerulonephritis (see Figure 3).
The most common causes of cryoglobulinemia, which included negative viral hepatitis serologies and an absent monoclonal spike on serum and urine protein electrophoresis, were ruled out. The ANCA was negative, along with negative titers for MPO and PR3.


