Risk Factors
Although the exact incidence is unclear, it’s now thought that scleroderma renal crisis affects around 2–15% of scleroderma patients, with typical onset within the first three to five years after diagnosis.12
Dr. Steen and other researchers have identified risk factors for scleroderma renal crisis. These include high-dose steroids, worsening skin symptoms, positivity for anti-RNA polymerase III antibodies and new anemia or cardiac events. Scleroderma renal crisis is also much more common in patients with the diffuse cutaneous form of the disease.12
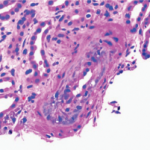
The presence of one or more of these risk factors can provide diagnostic clues about scleroderma renal crisis. Patients usually present with malignant hypertension but may also be normotensive (though with increased blood pressure from their personal baseline). Patients have rising creatinine levels, low urine output, and often have microangiopathic hemolytic anemia.12
Diagnosing scleroderma renal crisis can sometimes be a challenge, particularly if it is the first presenting symptom of scleroderma. It is sometimes misdiagnosed as thrombotic thrombocytopenic purpura, as hemolytic uremic syndrome or as atypical hemolytic uremic syndrome. Anti-neutrophil cytoplasmic antibody–associated vasculitis is another potential cause of acute renal failure in a patient with scleroderma, and it requires different treatment.12 But Dr. Steen notes, “Even if there is another possible diagnosis, I feel that if they have scleroderma, they should be treated with an ACE inhibitor until another diagnosis is confirmed, because it is both potentially kidney saving and lifesaving.”
Current management of scleroderma renal crisis requires early and aggressive intervention with ACE inhibitors and, if needed, with other medications, such as calcium channel blockers, and dialysis. Beta blockers should be avoided, because they exacerbate Raynaud’s phenomenon. If renal function has not returned within a year of continued ACE inhibitors, renal transplantation is the next step.12
Outcomes & Ongoing Research
Although the introduction of ACE inhibitors dramatically and positively changed outcomes of scleroderma renal crisis, some patients still do die or require long-term dialysis. In a study of 145 patients with scleroderma renal crisis treated with inhibitors, 38% of patients had poor outcomes.14 Older, debilitated patients and those with congestive heart failure also tend to do worse, as do patients presenting with greater than 3mg/dl creatinine.15 Dr. Steen explains, “Some of them don’t do well because they weren’t diagnosed promptly and accurately, and some don’t do well because the disease is so resistant.”
Dr. Steen emphasizes the need for both physician and patient education. Physicians need to be on the lookout for scleroderma renal crisis and recognize it as an urgent situation that requires immediate treatment. Particularly for high risk groups, it’s critical that patients understand the potential symptoms of high blood pressure, monitor their pressure at home and seek immediate treatment when necessary.
Since the advent of ACE inhibitors and the improved survival of renal crisis, lung involvement with pulmonary hypertension and pulmonary fibrosis has surpassed kidney disease as the leading cause of death in scleroderma patients.16 Yet scleroderma renal crisis still remains a major risk factor for mortality in scleroderma patients. After the initial improvement with introduction of the ACE inhibitors in the 1980s, the prognosis has not changed much.
Research continues for agents that might improve outcomes. Dr. Steen points out that it is difficult to perform good clinical trials of scleroderma renal crisis because the disease manifests so quickly. Researchers are currently exploring whether the addition of endothelin-1 receptor blocker medications—now used to treat digital ulcers and pulmonary hypertension in scleroderma—might also improve outcomes in scleroderma renal crisis when used in addition to ACE inhibitors.17