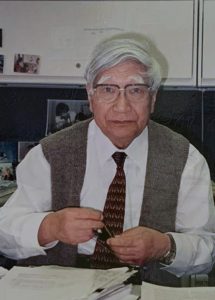
Japanese pediatrician Tomisaku Kawasaki, MD, who identified an inflammatory syndrome that affects children, died on June 5 in Tokyo. He was 95.
Tenacity & Attention to Detail
Born Feb. 7, 1925, in Tokyo, Dr. Kawasaki graduated from medical school at what is now Chiba University in Chiba, Japan, in 1948 and worked as staff pediatrician at the Red Cross Hospital in suburban Tokyo. It was there in 1961 that he saw his first patient with the disease that would eventually bear his name. Kawasaki disease has been in the news recently because some children testing positive for COVID-19 have exhibited comparable symptoms, including rash and extremely bloodshot eyes. “The connection between [the conditions] is a wide open question right now,” says pediatrician Jane Burns, MD, director of the Kawasaki Disease Research Center at the University of California, San Diego.
Dr. Kawasaki’s patient was a 4-year-old patient with unusual symptoms he could not diagnose. “The boy presented with a fever, congestion of the mucous membranes, cervical lymphadenopathy and desquamation,” says Philip Seo, MD, MHS, associate professor of medicine at the Johns Hopkins University School of Medicine, Baltimore, director of both the Johns Hopkins Vasculitis Center and the Johns Hopkins Rheumatology Fellowship Program, and physician editor of The Rheumatologist. “The patient eventually improved on his own and was discharged with the honest label of ‘diagnosis unknown.’”
Dr. Kawasaki subsequently had seven more patients with these unusual symptoms, which he documented in great detail and presented as a case series at a meeting of the Japanese Pediatric Association. When he submitted the series for publication, it was rejected; the reviewers suggested he had observed an atypical form of Stevens-Johnson syndrome.
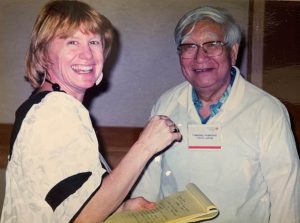
“There was almost an idea that because he was outside of the establishment, he could not possibly have described a new disease,” says Dr. Burns, who first met Dr. Kawasaki when she was a young infectious disease fellow and over the years came to consider him a dear friend.
During the next six years Dr. Kawasaki documented 50 similar cases of children with symptoms that included high fevers, extremely red eyes and lips, and a swollen red tongue, as well as swollen, peeling hands and feet. This case series was published.
“Maybe because he was unfettered by too much training, he could just see clearly what was in front of him,” says Dr. Burns. “Can you imagine today a rheumatologist waiting to report a new condition and gathering 50 patients over a period of years?”