The large vessel vasculitides were a major focus of the 21st International Vasculitis Workshop held in Barcelona in April. The biennial conference brings together specialists from multiple disciplines, including rheumatology, nephrology and immunology, to discuss cutting-edge vasculitis research. This article reviews important points regarding the pathogenesis, diagnosis and management of both giant cell arteritis and Takayasu arteritis.1
The large vessel vasculitides were a major focus of the 21st International Vasculitis Workshop held in Barcelona in April. The biennial conference brings together specialists from multiple disciplines, including rheumatology, nephrology and immunology, to discuss cutting-edge vasculitis research. This article reviews important points regarding the pathogenesis, diagnosis and management of both giant cell arteritis and Takayasu arteritis.1
1. Interleukin-17 and giant cell arteritis. Hélène Greigert, André Ramon, Baptiste Lamarthée, et al. Abstract O-005.
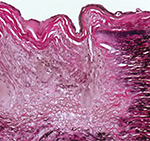
Although giant cell arteritis (GCA) is the most common form of systemic vasculitis in North America, our understanding of its pathogenesis is incomplete. Investigators from Dijon University Hospital and l’Université Bourgogne Franche-Comté, Dijon, France, ascertained the role of interleukin (IL) 17 in the pathogenesis of GCA using two different approaches.
In the first approach, fragments of temporal artery biopsies were cultured in the presence of IL-17, a monoclonal antibody directed against IL-17 (i.e., secukinumab) or pooled immunoglobulin. Using reverse transcription–polymerase chain reaction (RT-PCR), these investigators demonstrated that culturing temporal artery biopsies with IL-17 increased the expression of genes associated with vascular inflammation, T cell recruitment and fibroblast proliferation. However, culturing temporal artery biopsies with secukinumab decreased expression of many of these genes.
In the second approach, vascular myofibroblasts were isolated from healthy arteries and treated with IL-17, interferon-૪, secukinumab or a combinations of these agents, with the following results:
- Interferon-૪ induced expression of IL-17;
- IL-17 induced expression of genes related to vascular inflammation, leukocyte adhesion, and myofibroblast proliferation; and
- These changes were abrogated by exposure to secukinumab.
TitAIN was a phase 2 randomized controlled trial that demonstrated secukinumab may be an effective therapy for giant cell arteritis. This current study provides a mechanistic basis supporting the use of IL-17 blockade for the treatment of giant cell arteritis. Taken together with other studies (see abstract 2603, the evidence suggests secukinumab may become the treatment of choice for patients with giant cell arteritis who fail to respond to tocilizumab.2
2. Infections and incidence of giant cell arteritis. Lucas Pacoureau, François Barde, Alexis Elbaz, et al. Abstract O-014.
The etiology of giant cell arteritis is unclear. However, genetic associations imply that infection may play a role.
In this study, investigators analyzed a cohort of almost 100,000 women who have been followed since 1990. This cohort included 428 patients who had giant cell arteritis and/or polymyalgia rheumatica, who were compared with 8,560 matched controls.
Patients with giant cell arteritis had a higher risk of infection, which was most pronounced in the six months prior to their diagnosis of giant cell arteritis (odds ratio [OR] 1.62, 95% confidence interval [CI] 1.09–2.42). The same increased risk of infection was not observed among patients who had polymyalgia rheumatica alone.